Did you know that the skin is the body’s largest organ? It covers about 1.8 square meters!1 It serves as the body’s outermost protective layer by limiting the movement of molecules into and out of the body, holding all of the body’s organs close together, and being the first defensive barrier against foreign threats. But its effectiveness as a barrier presents some challenges when we want to get medicines to go through the skin into the body. Some new technologies are using nanoparticles to help get around those challenges.

The structure of the skin is key to how it works. It is made of three layers – the epidermis, dermis, and hypodermis – which among other things, give skin its durable and flexible qualities.1 (For more information on the makeup of the skin, see Alicia McGeachy’s blog post on what gold nanoparticles have to do with wrinkly skin.) The figure below illustrates the pores, hair follicles and sweat glands in these layers as the routes that control the movement of molecules into and out of the body. These molecules include water, salt, oils, and now drugs as we use the skin to act as a drug delivery system for treating different ailments.1

The direct application of drugs to the skin and their movement through the skin is called dermal drug delivery.1-4 Sunscreens, muscle rubs, acne and dermatitis creams are all examples of dermal drug systems, though some (like muscle rubs) are made to penetrate below the skin and others (like dermatitis creams) are made to stay the outside of the body.1 Drug delivery through the skin provides many advantages over other drug delivery routes such as oral (by mouth) or intravenous injection (into the bloodstream). One advantage of dermal delivery is that it is a pain-free alternative to syringes or hard-to-swallow pills. Dermally applied drugs have easy self-administration and easy removal if an allergic reaction were to occur. Unlike pills, dermal drugs also have the advantage that they do not require digestion in the intestines, but go straight into the bloodstream after passing through the skin so they will not cause negative intestinal reactions.1
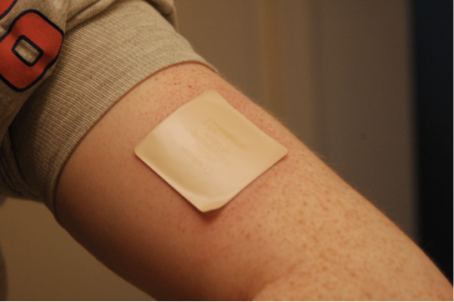
Although dermal drug delivery seems to be an ideal method for patients, designing drugs that are capable of being delivered through the skin is difficult. After all, one of the purposes of skin is to limit molecules from entering the body. So how can a drug manage to break through the skin barrier? Dermal drugs typically move between the cells in the epidermis layer of the skin.1 To squeeze past these cells, the drugs must possess certain characteristics. They must be very lightweight, have certain charge properties, and they have to be smaller than a few micrometers (millionths of a meter) so they can pass between the cell membranes.1
One way scientists have been exploring dermal delivery of drugs is by using nanoparticles. As you may remember, there are 1,000 nanometers in a micrometer, so nanoparticles definitely fit the size requirements for dermal drugs. The fact that they are so small generally takes care of weight restrictions, too. But just because a nanoparticle is small enough to go through the skin, does that mean that it will? How do scientists make sure that a nanoparticle wants to travel through the skin? It turns out that nanoparticles are also useful for drug delivery because they can be modified to fit the necessary charge characteristics.

One important characteristic is amphipathic behavior. Scientists design particles with both a polar (water-loving) region and a nonpolar (fat-loving) region. Amphipathic behavior allows nanoparticles to pass through the nonpolar epidermis membranes, and then be carried through the polar blood stream. (Remember the chemical rule: like dissolves like.)
Another aspect of charge on nanoparticle-delivered drugs is charge density. Charge density is the amount of electric charge on the particle’s surface per unit volume. If the drug is too positively charged, it may stick to the negatively charged cell membranes rather than traveling to its target. If the drug is too negatively charged then the cell membranes will repel the drug and that can also prevent delivery. So charge density has to be just right for the drug to pass between the cells.
Two more factors in nanoparticle design that are important for drug delivery are zeta potential and hydrophobicity. Zeta potential has to do with the electrical potential between molecules, and influences whether the particles remain stable or aggregate into useless or even painful clumps. Hydrophobicity is how much a particle “dislikes” water. A very hydrophobic drug will not dissolve in water, which means it will not be able to travel through the bloodstream, which is mostly composed of water. To avoid having the drug form painful clumps inside the body and to help it travel through the body to its desired target, the nanoparticle drug needs to be hydrophilic (water-liking).
There are a variety of dermal drug systems currently being developed using nanoparticles. One type of nanoparticle being investigated as a drug carrying system for dermal delivery is solid lipid nanoparticles (SLNs) (see below). SLNs are structures with lipid (fat) molecules on the outside and an interior area for carrying drugs.1-3 These particles can be made of physiological and biodegradable lipids that will passively move between cells because they are hydrophobic on the outside, just like the cell membranes they are passing.2,3 You can think of SLNs as camouflaged trucks: The truck seats are filled with drug molecules and their lipid surface camouflage helps them get past the lipids around the cells of the skin’s outer layer. Currently, SLNs are being implemented as drug delivery systems for some types of sunscreen, dermatitis conditions, hyperpigmentation, arthritis, and skin legions.2,5

Because they contain the drug completely inside their lipid shell, SLNs offer a solution for the problem of hydrophobic drugs that ordinarily would not be able to move through the bloodstream. In addition to transporting the drugs, SLNs protect the drugs from degradation until they reach their target.1-3 They can penetrate deeper into hair follicles than other dermal drugs because of their nano size.1 They can even be freeze-dried and stored for future use, allowing longer shelf life and easier transport of the drug from distributor to patient.2
These SLNs sound amazing, but there are some drawbacks. The lipids surrounding the particle may grow with time, transforming into a crystal lattice and gel that could prevent the release of the drug or even be toxic.1-3 There is also a drug loading capacity limit depending on the size ratio between the SLN and the drug.2,3 (Back to our camouflaged truck: you can only put as many people in the truck as there are seats and maybe floor space, right? The same with these SLNs. They have a limited inside area for carrying drug molecules, so you want to have as strong a drug as possible so the amount that fits in the SLN will be enough to do the job.)
Graphene patches are another drug carrying system under scientific investigation for use in dermal drug delivery. In June 2016, Hyunjae Lee and collaborators published a paper discussing the preparation of a graphene patch to be used for delivery of diabetes drugs (shown below).4 The patch has both sensor and drug delivery capabilities, meaning you only need the one device to both diagnose and treat the patient. The sensors measure temperature, acidity, humidity, and glucose concentration, which in turn send an electrical response to the drug delivery technology in the patch. The drug delivery component uses the electrical response as a heater to melt polymer microneedles loaded with the diabetes drug for delivery into the patient’s skin.4,6 In essence, when a patient’s glucose concentration changes, drug is delivered accordingly.

The advantage of this diabetes drug delivery system is that is more patient compatible than current technologies because the patient will no longer need to prick their finger for a glucose reading, the patch can detect the amount of drug the patient needs by measuring glucose levels, and it can stay on for automatic, immediate, and long-term detection and drug delivery. However, much like the limited ability of SLNs to carry large amount of drugs to intended targets, these microneedles can only carry small amounts of drug molecules, requiring a high potency drug to be really useful.4
The proposed and actual use of nanoparticles as drug delivery vehicles is becoming increasingly popular. They are being investigated to treat a range of disorders including diabetes, acne, eczema, and arthritis.1 Several different nanoparticle systems show promise in these applications including (but not limited to) the solid lipid nanoparticles and graphene patches discussed above, but also liposomes, silica, polymers and dendrimers.1,2 Further research into these drug delivering nanoparticles with a focus on drug affinity and efficacy will soon bring more of these patient compatible technologies to market.
EDUCATIONAL RESOURCES
- NISEnet: Nanomedicine in Healthcare Forum
- National Nanotechnology Infrastructure Network: Blood Glucose Monitor activity
REFERENCES
- Uchechi, O., Ogbonna, J. & Attama, A. “Application of Nanotechnology in Drug Delivery,” in Nanotechnology and Nanomaterials edited by Ali Demir Sezer. 2014. DOI: 10.5772/58672
- Kakadia, P. & Conway, B. Solid Lipid Nanoparticles: A Potential Approach for Dermal Drug Delivery. American Journal of Pharmacological Sciences, 2014, 2(5A), 1-7. doi: 10.12691/ajps-2-5A-1
- Wilczewska, A. et al. Nanoparticles as Drug Delivery Systems. Pharmacological Reports, 2012, 64, 1020-1037. doi: 10.1016/S1734-1140(12)70901-5
- Lee, H. al. A graphene-based electrochemical device with thermoresponsive microneedles for diabetes monitoring and therapy. Nature Nanotechnology, 2016, 11, 566- 574. doi: 10.1038/nnano.2016.38
- Yeh, M. et al. Dermal delivery by niosomes of black tea extract as a sunscreen agent. International Journal of Dermatology. 2013, 52(2), 239-45. doi: 10.1111/j.1365-4632.2012.05587.x
- Torrice, M. Graphene patch could help patients manage diabetes. Chemical &Engineering News, 2016, 94(13), 5. http://cen.acs.org/articles/94/i13/Graphene-patch-help-patients-manage.html
